What is Disc Prolapse and what is the Condition?
The spine is having 4 different spinal areas; cervical, thoracic, lumbar and sacral. The disc prolapses are commonly found in cervical and lumbar regions as these 2 areas are very mobile compared to the thoracic region.
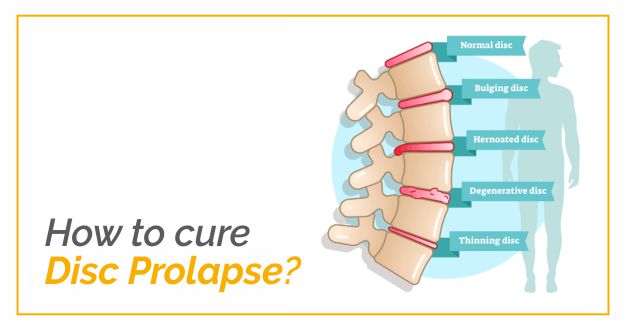
Mainly there are 2 types of disc prolapses
- Bulging disc
- Herniated or ruptured disc
The disc is having 2 different ring structures; annulus fibrosus (outer ring) and nucleus pulposus (inner ring) and post-injury or after degenerative changes in the spine, the disc may get damaged.
Bulging disc: When the outer ring is ruptured, the inner ring might bulge out posteriorly through the ruptured annulus fibrosus but still remain with the annulus fibrosus. This leads to bulging or protruded disc.
Herniated or ruptured disc: When the annulus fibrosus ruptures and the nucleus pulposus comes out of the annulus fibrosus; then the condition is called a ruptured or herniated disc. There can be disc extrusion or sequestered (free fragments) of the disc in the spinal canal. The herniated disc can compress the surrounding structures such as nerve roots; this can lead to pain radiating down the arm or leg (sciatica). The disc herniations can be of the following types: central, paramedian or mediolateral, lateral, foraminal and extraforaminal. Disc herniations are commonly seen especially on the MRIs, but these findings might not correlate with the clinical symptoms.
A study has found that nearly 30% of normal subjects showed disc prolapses on the MRIs, which makes MRI findings not highly reliable for diagnosing the disc prolapses. The cases of disc prolapse can be managed surgically or conservatively. In most of the cases, patients’ symptoms alleviate as the prolapsed disc moves back to its original position.
The disc prolapses (especially in lumbar region) are called massive if they occupy nearly 50% of the canal regions on axial MRIs after the prolapse has happened. The conservative management includes medicines, physiotherapy and injections etc.
Why does Disc Prolapse Happen?
There are various factors which can lead to disc prolapses and some of them are as follows:
- Age-related degenerative changes
- Severe injury or fall
- The sudden lifting of a heavyweight
- Repetitive forward bending or twisting movements
- Sedentary lifestyle or Obesity
- Poor posture maintained over a prolonged period of time.
- Tobacco smoking leading to a degeneration of intervertebral disc (IVD)
How Someone Avoids Back Surgery in Case of Disc Prolapse
As there is a high likelihood of the disc prolapse recurrence after the first episode, preventative care is important for the patients who are prone to get the disc prolapse. The major surgeries can be prevented and patients can be managed with minor surgeries after utilizing the benefits of effective physical therapy treatment plans.
Patient education plays an important part during the disc prolapse as most of the disc prolapses get better after some weeks. However, during this time, patients should maintain a good posture, use proper biomechanics especially while lifting, reduce body weight, avoid tobacco smoking and perform exercises regularly. The core strengthening exercises can be used to improve muscle activation and reduce the direct loading of the spine. However, if conservative management fails, surgery is the only option.
Should You Rely on Medications? What Could be the Side Effects?
Medications are mostly prescribed along with physical therapy for managing the acute disc prolapse cases. Medicines should be strictly taken under the direct supervision of a doctor. Various drugs can be prescribed in disc prolapse cases and almost all the drugs have associated risks and side effects. It is difficult to mention all the side effects and risks related to every medicine as the responses to medicines vary in every individual.
The commonest drugs used in disc prolapse are Nonsteroidal anti-inflammatory drugs (NSAIDs) and can lead to Edema (swelling of the feet), heartburn, stomach upset and stomach ulcers, increased risk of blood clots/ heart attack and stroke.
Opioids are another set of medicines used in disc prolapse cases and might cause symptoms such as constipation, drowsiness, nausea and vomiting, dry mouth and urinary retention. Next, steroids can be recommended by the orthopedic doctor and side effects such as weight gain, stomach pain, indigestion or heartburn, sleep problems, mood swings, bruising easily and skin thinning and stretch marks can be visible.
Lastly, muscle relaxants lead to drowsiness, fatigue, dizziness, dry mouth, depression, decreased blood pressure.
How does Physical Therapy Help in This Condition?
Physical therapy reduces the pain level, maintains and improves muscle activation, and relaxes the tight or spasmodic muscles. After disc prolapse, patients develop an altered pattern of neuromuscular functioning and physical therapy assists in improving or correcting these altered patterns.
Current research suggests that a person has to remain active during the initial weeks of prolapse and a physical therapist can be a great support for it and activities maintain good muscle and bone health. A therapist can use various modalities such as pelvic traction, ice or heat therapies and electrical stimulation to alleviate the symptoms. Along with that, patients are trained to perform the nervous tissue mobility, postural (listing) correction and conditioning exercises.
Patient education of proper biomechanics like holding the weight closer to the body and avoiding forward bending in the acute phase and controlling the body weight prevents the worsening of the disc prolapse.